01/04/2021 Empower Hour! Essential Oils
12/28/2020 Empower Hour! Homeopathy Review
12/21/2020 Empower Hour! Pain
SUMMARY: Tonight’s guest, Dr. Sheilah Robertson from Lap of Love veterinary home hospice, shared awe-some information about how you can help your pet have the best life. (more…)
12/14/2020 Empower Hour! Q&A
12/07/2020 Empower Hour! Hospice
11/30/2020 Empower Hour! Healthy Aging

Confused About Your Pet’s Symptoms, and Maybe Even Your Own? Gain Clarity With a Big Picture Perspective
Why our pets, or ourselves, for that matter, develop health problems can be a trickier question than it might appear. Say, for example, you take your puppy to the vet because you’re seeing symptoms that concern you. (And while we’re at it, let’s imagine that you take yourself to your doctor for the same reason.)
After running blood and stool tests on your puppy, your vet tells you, “It’s parvo. Your puppy was almost certainly exposed to it in the kennel.” After running blood tests on you, your doctor tells you, “It’s strep. You were almost certainly exposed to it at work.”
“But what caused it?” you ask, to which the vet responds, “The parvo virus,” and to which your doctor responds, “Strep bacteria.”
On your way home from the vet and doctor, you find yourself thinking, “The answers I was just given don’t make much sense to me. For one thing, my puppy’s litter mates were in the same kennel, exposed to the same virus, and none of them got sick. And as for strep, why has nobody else in my busy office gotten sick when I’ve been feeling awful for more than a week now?”
These are very, very good questions. Unfortunately, the answers that most people are used to receiving from both their vets and their physicians are purely circular. This is to say they essentially answer a question in a way that simply begs another question rather than shedding light on it.

The Confusion that is Created by an Incomplete Picture
 Have you ever heard the parable of the Blind Men and the Elephant. In it, five blind men each explore an elephant by touch. Depending on which part of the elephant they touch, they each believe that they are dealing with something entirely different: a snake, a rope, a spear, and so forth. They lack the vision to see the whole picture, and this leads them to draw false conclusions that, like the circular answers we just discussed, shed no light on the matter.
Have you ever heard the parable of the Blind Men and the Elephant. In it, five blind men each explore an elephant by touch. Depending on which part of the elephant they touch, they each believe that they are dealing with something entirely different: a snake, a rope, a spear, and so forth. They lack the vision to see the whole picture, and this leads them to draw false conclusions that, like the circular answers we just discussed, shed no light on the matter.
When your vet or physician tells you that an infectious agent (a germ, a bacteria, a virus, or even a gene) “caused” a particular illness or dis-ease, they’re working from a model that makes it very difficult to see the bigger picture. Without the bigger picture, you can’t gain an accurate understanding of the nature of the illness or dis-ease you are trying to address.
The term “causation” is misguiding. Living systems (like you and your pet) are what are known as non-linear, complex systems, or even more accurately, self-organizing systems. This means two things. First, everything that happens inside your body or your pet’s body is complex, which means that illness or dis-ease is not caused by a single isolated variable, or even a string of them. (That’s the non-linear/complex systems part.) Second, it means that your pet’s body, your body, and any living organism has an innate power to heal itself if adequate conditions can be created for supporting this process. (That’s the self-organizing part.)
If we are to speak of “causes” of health and dis-ease in any meaningful way that engenders clarity rather than confusion, we need a better way of seeing the bigger picture — of looking at health and dis-ease in context. By taking a look at the whole “elephant” and not just its parts, holistic perspectives and approaches can help us see the bigger picture and more fruitfully find our way forward.
Enter Holistic Perspectives and Approaches
The wonderful thing about holistic perspectives and approaches is that they transcend other approaches while including the best parts of them. In fact, one of the most effective ways to judge any approach across any discipline is whether it does a good job of respecting and reconciling the partial truths found in opposing views. Let’s take a look at how a holistic perspective looks when applied to Germ Theory.
You’ve probably heard of Louis Pasteur, the father of modern Germ Theory. According to this theory, certain illnesses or diseases are caused when the body is invaded by pathogens (“germs”).
But there’s another theory — a theory that may have been too ahead of its time to be adopted by the masses. This theory is called Terrain Theory (TT). According to TT, the internal system of an animal or person can be likened to a garden (or, more accurately, to an ecosystem). For pathogens to take root and breed illness or dis-ease, an ecosystem must be thrown out of balance to the point where it can no longer effectively defend itself.
The trouble with Pasteur’s theory is that it is too partial for making sense of why some pets and some people become ill when exposed to pathogens while others don’t. But when we add Terrain Theory to Germ Theory, a bigger picture emerges that confirms what may be research science’s most important maxim: correlation is not causation.
Gaining Greater Clarity
While this core maxim is not unknown to most vets and physicians, in actual practice, it is routinely ignored. This is unfortunate because if followed through to its logical conclusion, it can offer crucial insight for making critical distinctions that bear directly on treatment methods and modalities. It also helps us recognize why the answers we receive about causation often feel so unsatisfying and confusing.
While we may accurately say that a particular pathogen correlates with a particular illness, there is no logically sound reason to say that this pathogen causes it. Saying that a pathogen or pathogens cause a disease is like saying that the parts of an elephant cause the elephant, or that baseball players cause baseball games, or that children cause a family. Intuitively, this makes no sense, but when it comes to how we think about health, we’re so used to having correlation confused with causation that we rarely register the disconnect.
Seun Ayoade, a preeminent holistic thinker working from a hybrid model of Germ Theory and Terrain Theory, aptly points out the most complete and accurate predictor of dis-ease lies in investigating the relationship between multiple variables. The severity of an infection, he explains, depends on both the virulence of a pathogen and the condition of the complex inner terrain.
Said differently, It is in the interplay between complex variables —- the current condition of the inner terrain, germs, genes, diet, activity levels, social connections, emotional well-being, and forth — that we can find greater clarity for getting to the bottom of what’s ailing us and our pets and taking effective holistic action.
Leaving You and Your Pet Better Off Than Before
When I was growing up, I was taught to leave things better than when I found them. For example, I was taught that if I noticed litter on the street, that I should pick it up, or if I noticed a person who appeared to be down, that I should do my best to lift their spirits. This teaching has served me well and guided my own holistic journey.
Holistic approach aims at promoting vibrant health by restoring inner balance and increasing vitality.
The beauty of holistic actions is that they are designed to leave you and your pet better off than before you became ill or experienced dis-ease. This is because a holistic approach aims not merely at eliminating symptoms, but at promoting vibrant health by restoring inner balance and increasing vitality.
A holistic approach never says, “Let’s give your dog an antibiotic or two (or three) to get rid of that nasty pathogen, and never mind about her lack of exercise, poor diet, and the fact that she’s not getting enough social interaction. And oh, also don’t worry about the way that anti-biotic use will further compromise her body’s ability to protect itself from pathogens.”
A holistic approach says, “Let’s look at what your dog’s allergy symptoms may be trying to tell us about deeper issues that are going on in her system. Let’s look at her diet, her activity levels, her social interaction, and her sense of safety. Let’s see what other clues we might be missing by taking a thorough inventory of potential symptoms that are so subtle we may be missing them.
Let’s introduce pro-biotics to her diet and begin fresh feeding to help rebuild her system so she’s better able to defend against pathogens and more resistant to dis-ease. Since this isn’t an acute or urgent issue, let’s take our time to deeply understand what’s going on and to address it gently yet thoroughly before electing to use aggressive approaches like drugs or surgery. Let’s aim for inner balance and greater vitality and optimal health to give her the life she deserves.”
Which approach do you prefer?
Want Even More Support for Taking Holistic Actions to Promote Optimal Health?
Pet parents and holistic veterinarians around the globe are already using our holistic perspective and approach to nurture optimal health for their companion animals. If you’re a pet parent, you can confidently take easy holistic actions to increase your pet’s inner balance, protect them from pathogens, and enhance their quality of life. These free, simple and 100% safe lifestyle tweaks can be easily implemented through The Terrain Optimizing Protocol.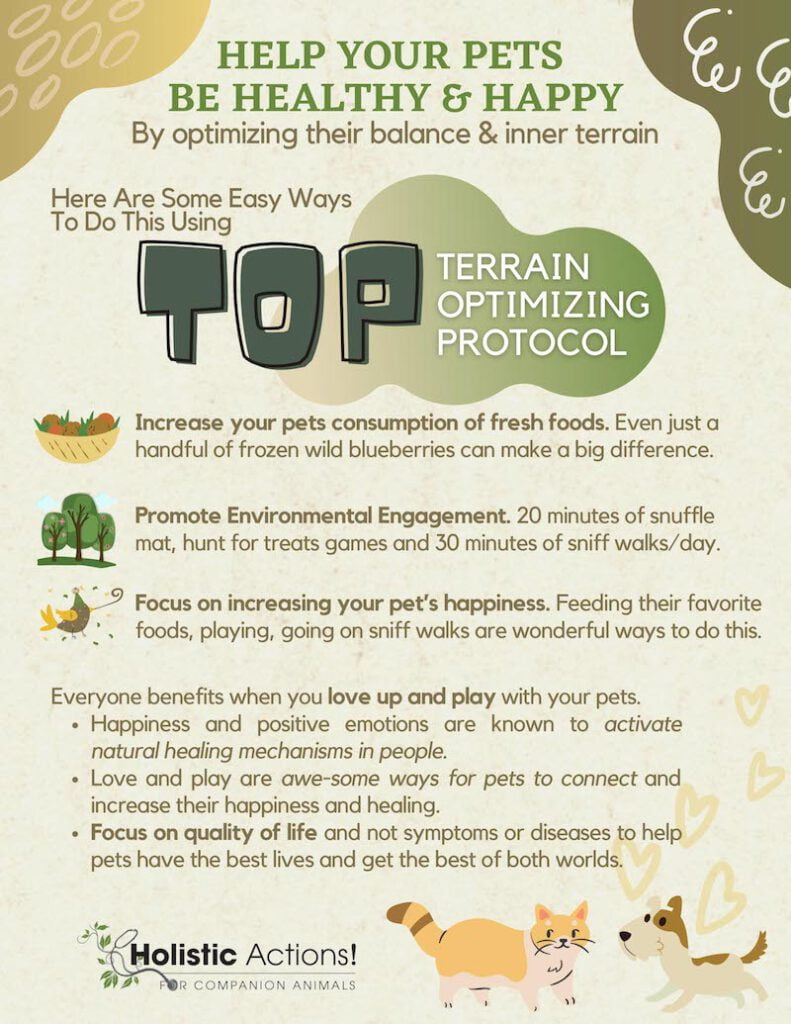
You’ll love the way it supports and fuels the natural healing ability of your pet’s body.
Holistic Actions! helps you get a big picture view of your pet’s symptoms to gain greater clarity about how to nurture optimal health.
Thank you for visiting us here at Holistic Actions! We wish you the best of luck on your holistic journey!
With care,
Dr. Jeff

How to Listen to and Learn From Your Pet’s Symptoms to Take Effective Holistic Action
Learning to view your pet’s symptoms as trustable, intelligible communications that can provide clues to underlying imbalances and guide holistic health interventions is one of the most important things you can do.
This is often a difficult task, since almost all of us have been conditioned to view symptoms as an enemy that we must medically defeat. But symptoms are not our enemy but our ally, and this reversal of perspective is one of the most rewarding you can take; not only for your pet’s life, but for your life.
When your pet’s symptoms are not viewed as something to fear but as something valuable to which you can listen and from which you can learn, it quickly becomes apparent that they offer a breadtrail to the very solutions you are seeking — holistic actions that don’t just cover up or quiet down symptoms, but that create new levels of inner balance and vitality to make your pet’s system even more resilient against dis-ease.
A Quick Word About the Difference Between Signs and Symptoms
It bears noting here that what we’re calling in this article “symptoms” are understood medically as “signs.” Technically, symptoms refer to indications of distress or dis-ease that are subjective and therefore invisible, such as the particular quality of pain or the experience of having a nightmare.
Because animals aren’t able to tell us about symptoms, we must technically go on signs. Signs are indications of distress or dis-ease that may not be outwardly visible, such as elevated white count, fever, and so forth. Another way to understand the difference between symptoms and signs is that the first is subjective and the second is objective. But for the purpose of this article, we’re just using a single term — symptoms — to refer to both.
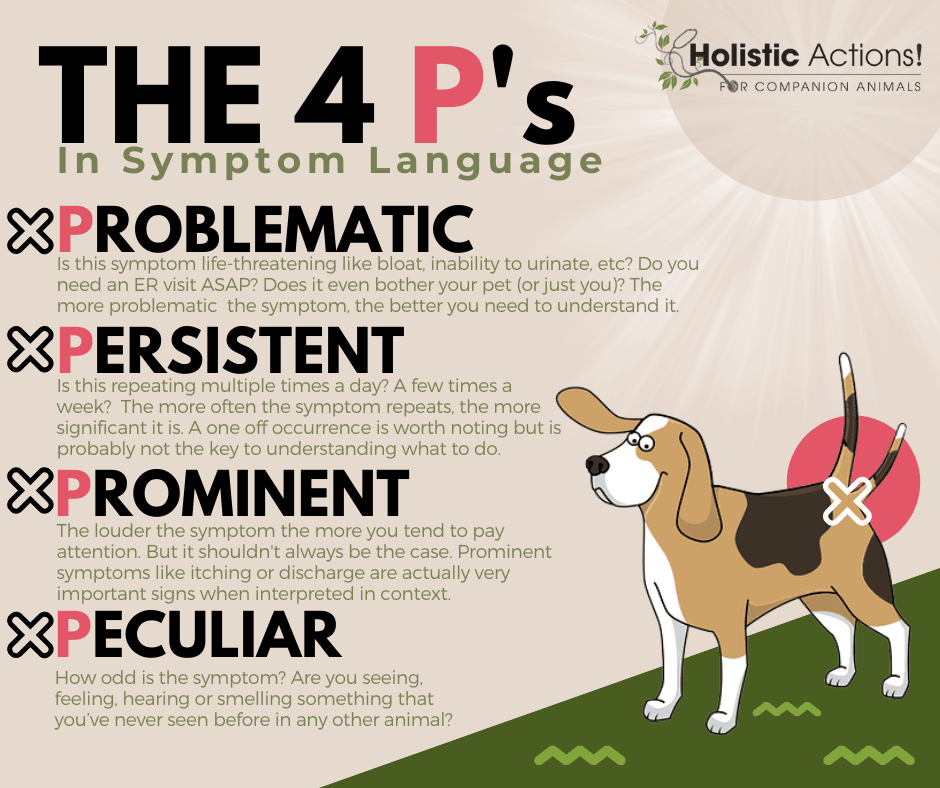
The real question now is how you can have a “conversation” with your pet by listening to their symptoms in order to learn from them? The 4 P’s methodology we’re about to teach you will give you tools for doing this and transform your capacity to respond appropriately to what your pet’s system is telling you.
Without Further Ado…The 4 P’s!
The 4 P’s offer a listening framework to help you approach symptoms with the right mindset and the right questions.
- Pay attention to Problematic symptoms: Health challenges that may limit your pet’s life, like obesity or chronic allergies.
- Pay attention to Prominent symptoms: Those that most loudly say, “Pay attention to me!” Acute dis-ease symptoms fall into this category.
- Pay attention to Persistent symptoms: How often do you see the symptom? Hourly symptoms are usually more significant than weekly.
- Peculiar Symptoms: Have you ever seen this symptom before in your pet or anyone’s pet or does it strike you as particularly odd or usual?
And here’s two other P’s that help you work with your pets bodies and symptoms and not suppress them:
- Approach symptoms with Patience: Deep and permanent healing occurs slowly.
- Approach symptoms with Perseverance: You might need a new approach or different (not just a second) opinion. Don’t give up!

BEAM — Another Helpful Framework for Listening to and Learning from Your Pet’s Symptoms
BEAM should be improving over time.
This basic BEAM model of four symptom categories provides an additional framework for understanding and assessing symptoms. BEAM stands for Behavior, Energy, Appetite, and Mood. The Beam models helps shine the light on optimal long term health and to provide an overarching context for viewing symptoms.
When it comes to holistic strategies for your pet, BEAM should be improving over time. It’s extremely important to track changes in BEAM symptoms, especially if they are Prominent, Persistent, Problematic or Peculiar.
So ask yourself, which categories do my pet’s symptoms fall into? The more categories in which symptoms appear, the more urgent is the need for intervention to restore or improve your pet’s inner balance and vitality.
Symptoms that Change In Response to Environmental Changes (“Modalities”)
Pay especially close attention to symptoms that change depending on the context. They are among the clearest communications you will receive from your pet’s system. These symptoms may appear…
- When you get ready to leave the house or come home from work, with your pet becoming especially clingy or needy, or going off by themselves at specific times of day or night.
- In weather conditions like heat, cold, rain, wind, etc.
- During or after: eating, drinking, waking, defecating, urinating, etc.,
- In relation to certain foods. (Fresh feeding of a variety of foods makes symptoms like this much easier to recognize.)
- And more!
Symptoms that occur at the same time, or what are known as concomitant symptoms, can also be very significant. For example vomiting along with diarrhea, increased drinking along with sneezing, etc.
Additional Considerations and Questions for Collecting Clues
Keep a daily log of symptoms and carefully record any changes, no matter how seemingly insignificant. Changes in your pet’s usual patterns and habits as viewed through the BEAM model are especially significant, even if they appear to you to have nothing to do with your pet’s problem. Where relevant, record the answers to the following questions in your log to collect the clues you need for helping your pet.

- When did the problem begin and what circumstances were associated with it or may have brought it on?
- Have there been previous illnesses such as ear and eye “infections”, allergies/skin diseases, colds, skin growth removals, urinary problems, etc.?
- Specifically, which treatments were used, for how long and what doses were any drugs used? What were the results?
- How about new symptoms associated with a medication (no matter how benign you were told that it is)?
- Are there any conditions that started along with the main problem you’re concerned about?
- Is there a time of day, night, month, or season that the symptoms are better or worse? Are they better or worse before or after eating, sleeping, moving, resting, or when your pet is occupied with a favorite activity? (Anything that makes the symptoms better or worse is extremely important to note.)
- Do symptoms appear at a specific time, season, phase of the moon, temperature/barometric pressure etc.? For example, is joint stiffness worse when it is humid?
- Do the symptoms remain the same or do they change character or shift from place to place?
Narrow Your Focus to Gather Even More Clues!
The real breadcrumbs to the solutions you’re seeking are found in the details! By focusing on the following areas, you’ll be led that much closer to the right holistic actions to take for your pet!
APPETITE
- How is your pet’s appetite? Does she beg for food and always appear hungry? Is there an increase or decrease in appetite?
- Does your pet’s appetite seem excessive or are they inexplicably picky?
Does your pet seem preoccupied with particular kinds of food or with particular flavor profiles or textures? (Salty, sweet, fatty, sour, spicy, egg-like, or ice cubes?) - Does your pet trying to eat non-digestible items like dirt, rocks, sand, stool, pencils, etc.?
- Is your pet fed in a crate, and if so, why?
- Does your pet eat out of a bowl or need to be hand-fed?
- How fast does your pet eat? Does she take a few bites or eat all of the food right away?
BEHAVIOR
- Have there been behavioral changes such as being easily startled or starting from sleep or seeming sensitive to being touched?
- Do these behavioral changes improve or worsen with diversion such as a walk or car ride? Is your pet’s reaction to you opposing certain behaviors (like jumping up on somehow) any different than usual?
- Is your pet behaving differently with guests or interacting with strangers in ways you’ve never before witnessed? Does your pet actively avoid interaction or retreat to a room by themself to seek solitude?
- Has your pet become more or less reactive to small animals, other dogs or people? How long after an encounter with one of these does reactivity occur? Is it expressed through jumping, lunging, barking, growling, trembling, or cowering?
- Does your pet appear restless or unable to settle down?
- Do they suddenly begin to avoid hard surfaces or seek out hard surfaces to lie on, and rest in positions they have not favored before?
- Do they prefer sun or shade more frequently than normal, or do you notice unusual or extreme behavior changes in relation to temperature changes?
- If your pet is involved in any kind of training, do you notice an increase or decrease in focus, a change in excitement level or loss of motivation in response to using food, toys, and praise as a reward?
- Do you notice a sudden reluctance to sit, heel, etc., or a sudden change in your pet’s attitude toward training?
- Is your pet vocalizing and/or moving in their sleep in ways you’ve never seen before? If so, are you seeing whining, barking, snoring, paws or legs twitching (all paws?), or they’re legs moving as though they are running?
BATHING, BRUSHING, PETTING, AND GROOMING
- Does your pet suddenly no longer want to be brushed or pet or seek out brushing or petting when having avoided it in the past?
- Do they suddenly react to brushing or petting in an unusual way such as spinning, whipping their head around, trying to bite you, moving head from side to side, licking the air, or “dancing” with back legs?
- How does your pet react to running water? Does your pet suddenly avoid baths or resist getting out of the bath?
- If your pet is a cat, has their been a reduction or cessation of grooming?
COAT
- Is your pet losing unusual amounts of fur or shedding at unusual times? If so, is the hair falling out evenly or in bunches or tufts?
- Do you note dandruff, dry or brittle fur, a change in your pet’s coat in terms of thickness, shine, dullness, or oiliness?
DISCHARGE
- Discharge details are very important. Are you noticing any discharge from our pet’s nose, eyes, or sex organs? , Is it scant or copious, thick or thin, or sticky? What is the color and odor? Does it appear to be causing irritation to the tissues it’s being discharged?
FEMALE CYCLE
- If your pet is an intact female; how old was she when she first came into heat, how far apart are the cycles, are there any behavior changes or physical symptoms that accompany heat?
- What does the vaginal discharge before, during, and after the heat cycle look and smell like?
- Has she ever been pregnant? Did she breed and conceive easily?
- How did she carry, any problems delivering?
- Did she have plenty of milk? Were there any problems associated with nursing?
LAMENESS AND EASE OF LYING DOWN AND GETTING UP
- Is your pet favoring or protecting a specific foot or holding her paw up?
- Do you notice soreness or swelling to the paw or legs, and when it is genty pressed on, does an indentation occur, and if so, for how long does it stay before returning to normal?
- Does the swelling feel soft or firm, an dis it hot to the touch?
- Does your pet exhibit pain with rotation of what appears to be an afflicted joint?
- Can your pet lie down and get up quickly and easily? Do they lie down with their back legs or front legs first?
- Do they yelp or cry out when they lie down, spin prior to lying down?
- When they lie down, does their back end go down fast but front end slow?
- Does your pet yelp or cry out when getting up or attempt to use a wall or some other source of support for standing?
MASSES | GROWTHS
- Do you notice any masses or growths on your pet? What is the size of these growths? Are they open and expelling fluid or bleeding or emitting odor?
- Are masses soft or hard, painful, and movable?
- Have their been any changes in the shape, size, or growth-rate of a mass?
RESPIRATORY
- Does your pet pant excessively or have trouble breathing?
- Is your pet coughing? If so, what does the cough sound like? (Hacking, rasping, wheezing, wet, or dry?)
- What is the frequency of your pet’s coughing, the time of day it occurs, and the duration of the coughing episode?
- Does the cough coincide with or seem to be triggered by waking up, when on-leash, or after eating or drinking?
- Is your pet sneezing? If so, what is the frequency, time of day, triggers, length of the sneezing episode, and how many sneezes in a row do you count?
SKIN
- Do you note any skin changes or lesions? What is their exact location and color? Are they dry or moist, thick or thin, scaly, or pimply? Are their warts or other growths? Are they dry, flaky, powdery, red or inflamed?
- What about open sores, clogged pores or cysts, or changes in skin pigmentation? What is the appearance of skin overall?
- Is the skin itchy and does your pet seem to get relief from scratching or does that seem to make it worse? Does heat, cold, exercise, wearing a collar, etc., make it better or worse?
STOOL | GI SYMPTOMS
- Does mucus or blood appear in the stool? Does defecation coincide with waking, eating, drinking, etc.?What is the frequency and urgency of defecation? (Does your pet rush to the litter box or to the door at a certain time of the day?)
- What is the odor, color, and consistency of stool? Are the stools very smelly (do they burn your eyes from 6 feet away?). Are they hard, dry, large, pasty, bloody, frothy, slimy, thin, watery, slender, or flat?
- Normal stools are well-formed and are easy to pick up (and don’t leave mush on the ground).
- Soft-formed stools may look the same (or a bit wetter) but are harder to clean up
- Pudding stools are the consistency of soft serve ice cream.
- Watery stools are in liquid form.
- Does stool shoot out like water from a hose with (or without) gas? Is there straining before, during, or after passing stool? Does your pet continue to try and eliminate even after they have defecated? Do you hear (or smell) gas before, during, or after passing a stool? How about noises from the stomach?
THIRST
- Is your pet drinking less or more than usual? Is there thirst for large quantities at one time, small frequent quantities, or little thirst?
- Is there a preference for cool fresh water vs. room temperature or warm water? Is there a preference for water that comes out of the tap, backyard hose, or bathroom toilet?
- Is your pet a “sloppy” drinker? (Does the water go all over the place after a drink?)
URINE
- What is the color, how frequent or urgent is the need to urinate?
- Have there been any accidents or periods of incontinence?
VOMITING OR REGURGITATION
- Is vomiting active or passive? Does vomiting seem painful to your pet? Is there retching?
- What is the vomitus odor, amount, color, and consistency? (Foamy/frothy, lumpy, liquidy, etc.)
- Do there seem to be identifiable food triggers, activity-related triggers, or specific times of the day you witness vomiting? Does it seem in any assoicated with, drinking, going out or coming in, or defecating?
- Do you notice weakness after vomiting?
SEXUAL ISSUES
- Do you notice any male or female sexual issues? Trouble breeding, masturbation, excessive mounting behavior, or penile or vaginal discharges related or unrelated to heat?
The More Clues You Collect, the Better Off Your Pet Will Be!
Holistic Action is here to help you interpret your pet’s symptoms and use them as a trustable guide for taking effective holistic actions — actions that don’t just cover up or quiet down your pet’s symptoms, but that create new levels of inner balance and vitality to give them the happy, healthy life that every dog and cat deserve!
Thank you for visiting us here at Holistic Actions! We wish you the best of luck on your holistic pet care journey!
Be well.
Dr. Jeff
11/23/2020 Empower Hour! Homeopathy|Evaluation of Response

Faced With Making a Medical Decision for Your Pet? Push “Paws” to Ensure a Fairy Tale Ending
Once upon a time, not so very long ago (in the last year, actually), there was a beautiful, golden-haired girl named Sam. Sam’s energy, enthusiasm, and love of cuddling brought joy to everyone who knew her, especially her parents. Sam’s parents took a holistic approach to caring for her. Not only did they consider and care for Sam’s physical health, but also her emotional, social, and energetic wellbeing.
Sam’s parents fed her a variety of fresh foods in just the right combinations and portions to ensure optimal nutrition and weight. Sam was minimally vaccinated, and in her seven years on earth, had only minor health challenges, such as eye redness and ear discharge that were treated by the local veterinarian. (If you haven’t guessed it by now, Sam is an adorable golden retriever.)
But when Sam suddenly began drinking much more than usual, the fairy tale that Sam and her pet-parents seemed to be living almost came to an end.

A Small but Highly Significant Symptom
Even though nothing else seemed amiss, when Sam’s parents noticed this sudden change in her behavior, they immediately scheduled an appointment with Sam’s veterinarian.
Sam’s parents were committed to getting the best treatment for Sam, though at this point, they weren’t yet sure what the problem might be. But they also wanted to do the best for her.
At the vet, nothing of note was found during Sam’s examination, so the doctor drew some blood and collected some urine to be sent out to the lab for testing.
Sam was sent home with anti-biotics, with instructions to administer them twice daily. Intuitively, something about this didn’t sit right with Sam’s parents, so they decided to wait until further test results came back before taking action.
The Plot Thickens
Two days later, the vet called with the test results. Everything looked fine except for one elevated enzyme called the serum alkaline phosphatase (SAP).
The test result, he said, was just a clue to what was happening in Sam’s body and nothing to worry about.
The vet told Sam’s parent’s that her increased drinking and SAP could be early signs of Cushing’s dis-ease. The test result, he said, was just a clue to what was happening in Sam’s body and nothing to worry about.
He recommended that Sam be seen in six months for reevaluation, and encouraged Sam’s parents to begin the antibiotics he’d prescribe for her, “just in case of a hidden infection,” assuring them this course of action couldn’t hurt anything and might actually help in some way. Once more, this advice didn’t sit right with Sam’s parents.
Sam’s Parents Push “Paws”
Pushing “paws” means being mindful, and being mindful means taking the time to look deeper, to put yourself in a position to skilfully respond rather than blindly react. Sam’s parents were mindful before proceeding with the recommendations they’d been given.
This is a critical step before making any medical decisions for non-life-threatening problems. It involves research into potential treatment interventions, unbiased education on alternative models of health,, and networking with other pet parents and professionals. In most cases, it will also involve obtaining a second (and in many cases, a third) opinion from a holistic clinician on the accuracy of a diagnosis and the wisdom of pursuing a particular treatment option.

A Different Way of Looking at Things
Sam’s parents had been scouring the internet for insight into her symptoms and how they could potentially be interpreted in ways that differed from the opinion of their vet. One of the things that stood out to them was an approach that promoted proactive prevention rather than reactive treatment.
In other words, what had caught their attention was the idea that getting Sam the best treatment possible wasn’t just about addressing her symptom and keeping an underlying problem at bay, but rather about promoting the healing power of Sam’s own system. This approach was about creating a whole new level of balance and vitality for Sam that would not only improve the quality of her life but also make her much more resistant to any form of dis-ease.
Sam’s guardians approached their vet about taking a closer look at Sam’s symptoms to perhaps generate some alternative explanations for what might be going on. The vet once more assured them they had nothing to worry about. “But,” he told them, “if it will make you feel better, you can consult with an internal medicine specialist.” With that, Sam’s parents made an appointment for the following week.
After the consultation with the internal medicine specialist, the internist agreed that a better understanding of Sam’s problems was indicated. But since the examination yielded no new clues, further diagnostic testing was needed. The testing costs in this case would run $650. “Hopefully,” the internist told them, “they will be useful.”
The Dawning of New Realizations
Because Sam’s parents had been doing their homework and had been exposed to a new way of thinking, they returned home with some dawning realizations. Though they weren’t sure what the next steps might be for Sam, many new things were suddenly registering for them. First and foremost, they registered that the clinicians they were working with were limited to a very narrow model of health. This model looked at symptoms and solutions in a very “cookie-cutter,” “paint-by-numbers” fashion.
They didn’t look at the bigger picture of Sam’s life.
Those working from this model seemed to have no awareness of, or at least no trust in, the wealth of clues that could be collected by bringing the right questions to bear. In short, they didn’t look at the bigger picture of Sam’s life. It lacked robust information-gathering protocols to guide individualized treatment approaches and comprehensive treatment plans.
It also struck Sam’s parents for the first time that it was odd that they, those closest to Sam who knew her best, were not looked at as collaborative partners in discovering what was really going on with Sam. In fact, it put them in a passive position that often brought them to the verge of feeling powerless. Last, they realized that this narrow model looked at Sam’s body like a broken machine that needed to be fixed with drug-based tinkering rather than a living system with immense intelligence and self-healing capacity that needed to be tapped.
Sam’s parents realized that if they weren’t careful, the interventions they were being prescribed had a good chance of making whatever was really going on with Sam even worse, putting them on a “misery-go-round” of ever-worsening symptoms and increasingly aggressive interventions, including surgery. This wasn’t a ride they were willing to take.
Sam’s Parents Take “The Road Less Traveled”
The parent of one of Sam’s friends had just consulted about some of her own concerns with a conventionally trained but holistically and homeopathically-oriented vet in another state. Though it seemed odd to Sam’s parents that their fellow pet parents had consulted with a vet in another state with such unusual credentials, they’d come to the point that they were ready to look for help in new places.
When Sam’s parents consulted with this vet, they couldn’t believe the difference between the integrative, holistic approach he offered, and the narrow model they’d always encountered. Not only did they feel like they were being looked at as active collaborators rather than passive participants, they felt that Sam’s innate healing power was finally being taken seriously in a way that could ensure her happiest, healthiest life and future.
The holistic vet assured them they could trust both external (outwardly visible) and internal (inwardly detectable via medical testing) symptoms. Together, he explained, these symptoms could provide reliable clues that could be accurately interpreted to guide sound holistic actions and effective treatment interventions. He provided extensive yet easy-to-understand information-gathering protocols for collecting clues that, with his professional support, could enable Sam’s parent’s to promote the healing power of her own system.
Not only did they feel like they were being looked at as active collaborators rather than passive participants, they felt that Sam’s innate healing power was finally being taken seriously in a way that could ensure her happiest, healthiest life and future.
This approach left Sam’s parents feeling more empowered and hopeful than ever, but the question remained, would it actually help Sam?
Sam’s Parents Take Holistic Actions on Sam’s Behalf
Remember Sam’s elevated SAP levels that Sam’s conventional vet told her parents could be early signs of Cushing’s Disease? A primary treatment goal for Sam was to naturally normalize her SAP and reduce her excessive drinking. (Since the excessive drinking was a clear sign that her system was out of balance.)
Using the information-gathering protocols they’d been given and professional support from the holistic vet, this collaborative effort led to an individualized treatment plan for Sam. Based on clues from Sam’s own body about how her system was responding, her progress was monitored and adjustments were made as necessary. Four months later, when Sam came in for her semi-annual wellness check, she was doing incredibly well. Her externally observable symptom of water consumption was back to normal, and her internally detectable symptom of elevated SAP was dramatically reduced.
You and Your Pet Can Have Your Own Happy Ending
Everybody wants a happy ending! Just like Sam and her parents, you can promote the immense healing-power of your pet’s own system. You can confidently do this without the use of toxic drugs, unnecessary surgery, and other aggressive interventions that run very real risks of generating even worse dis-ease in an attempt to treat it. By learning to trust your pet’s internal and external symptoms and use them as reliable clues for taking holistic action, you and your pet are that much more likely to have many happy, healthy, wonderful years together.

