
Ask A Vet – Live Q&A 6/27/25
If your pet is stuck in a cycle of symptoms and short-term fixes, this is the conversation you need to hear. Join holistic vets Dr. Christina and Dr. Jeff as they break down how to approach pet health differently—by decoding symptoms, understanding energy imbalances, and tracking what actually works for your unique animal.
Would You Like to Join Our Next Public Q&A Webinar?
We hold them every LAST Friday of the month.
Sign up below to get notified about the next session.

Dr. Christina
Christina Chambreau, DVM, is an internationally known homeopathic veterinarian and associate editor of the Integrative Veterinary Care Journal, she’s written several books on animal healthcare.
After opening her own homeopathy veterinary practice in 1983, she founded the Academy Of Veterinary Homeopathy and was on the faculty of the National Center for Homeopathy Summer School for ten years.
Dr. Christina is also an integrative medicine adjunct faculty liaison for the Maryland Veterinary Technician Program and lectures on a wide array of topics including integrating holistic options into veterinary practices, as well as guidance on how to choose the best approaches to heal animals and sustainability.

Dr. Jeff
Jeffrey Feinman, BA, VMD, CVH, graduated in 1985 from the University of Pennsylvania and was Penn’s first veterinary dual-degree University Scholar, holding both molecular biology and veterinary degrees. He is the founder of HolisticActions.com and dedicated to pet parent empowerment.
Dr. Jeff is devoted to researching about how to harness the innate power of the individual using Vitality and Balance. He and his wonderful wife Amy live with Archie, a rescue pup, and a Rex cat named Tigger.
06/23/2025 Empower Hour! Enhancing Shelter Care Through Animal Reiki
06/16/2025 Empower Hour! Bio Music One
06/09/2025 Empower Hour! EFT and Animal Communication in Shelters for Animals and People
06/02/2025 Empower Hour! Heart-Centered Healing for Shelter Animals and Their Caregivers

Ask A Vet – Live Q&A 5/30/25
If your pet is stuck in a cycle of symptoms and short-term fixes, this is the conversation you need to hear. Join holistic vets Dr. Christina and Dr. Jeff as they break down how to approach pet health differently—by decoding symptoms, understanding energy imbalances, and tracking what actually works for your unique animal.
Would You Like to Join Our Next Public Q&A Webinar?
We hold them every LAST Friday of the month.
Sign up below to get notified about the next session.

Dr. Christina
Christina Chambreau, DVM, is an internationally known homeopathic veterinarian and associate editor of the Integrative Veterinary Care Journal, she’s written several books on animal healthcare.
After opening her own homeopathy veterinary practice in 1983, she founded the Academy Of Veterinary Homeopathy and was on the faculty of the National Center for Homeopathy Summer School for ten years.
Dr. Christina is also an integrative medicine adjunct faculty liaison for the Maryland Veterinary Technician Program and lectures on a wide array of topics including integrating holistic options into veterinary practices, as well as guidance on how to choose the best approaches to heal animals and sustainability.

Dr. Jeff
Jeffrey Feinman, BA, VMD, CVH, graduated in 1985 from the University of Pennsylvania and was Penn’s first veterinary dual-degree University Scholar, holding both molecular biology and veterinary degrees. He is the founder of HolisticActions.com and dedicated to pet parent empowerment.
Dr. Jeff is devoted to researching about how to harness the innate power of the individual using Vitality and Balance. He and his wonderful wife Amy live with Archie, a rescue pup, and a Rex cat named Tigger.

05/19/2025 Empower Hour! 5 Element Archetypal Balance and Behavior
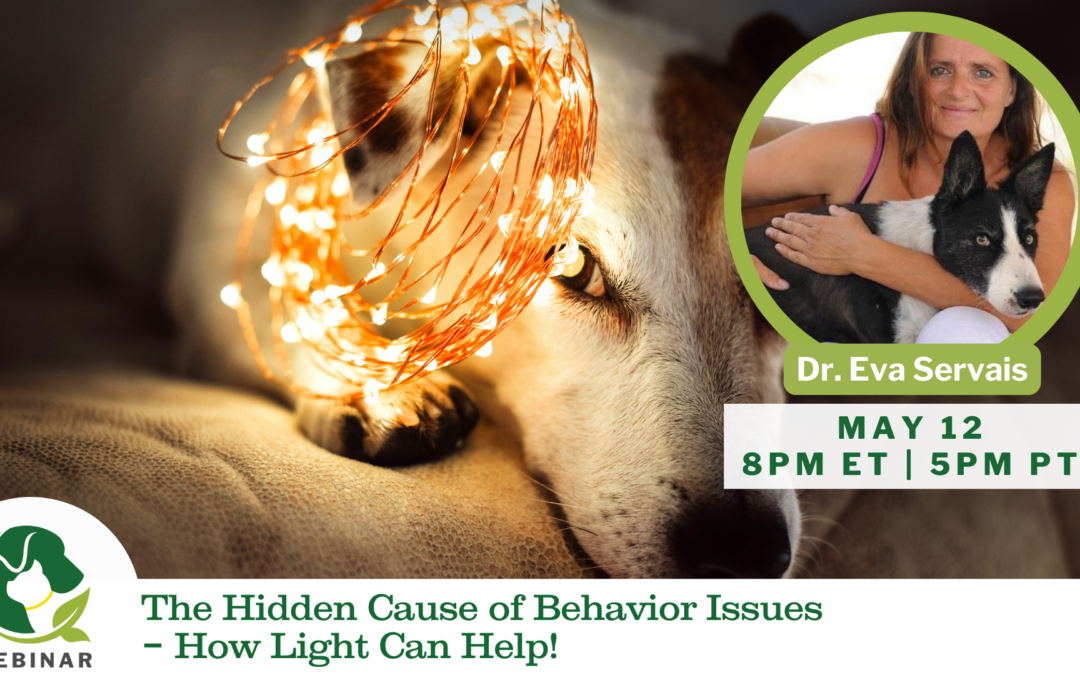
05/12/2025 Empower Hour! Light Therapy
05/05/2025 Empower Hour! Breath and Training

Ask A Vet – Live Q&A 4/25/25
If your pet is stuck in a cycle of symptoms and short-term fixes, this is the conversation you need to hear. Join holistic vets Dr. Christina and Dr. Jeff as they break down how to approach pet health differently—by decoding symptoms, understanding energy imbalances, and tracking what actually works for your unique animal.
In this session, we explored a range of powerful insights to help you think like a holistic vet:
🔹 Not-So-Picky Eaters – How letting your pet guide their food choices taps into their natural healing instincts.
🔹 Fermented Foods 101 – Why holey cabbage is gut gold and how simple ferments can transform your pet’s microbiome.
🔹 Food Energetics Made Easy – Discover how the thermal nature of foods (warming, cooling, neutral) can balance behavior and vitality.
🔹 Gut–Brain Connection – What you feed affects more than digestion—it influences mood, energy, and behavior.
🔹 Trusting Your Pet’s Wisdom – Dr. Provenza showed how animals can self-medicate when we let them listen to their bodies.
🔹 From Confusion to Confidence – Ditch the diet dogma and focus on what feels right for your pet—fresh food, loving connection, and tiny steps that stick.
🔹 You’re Not Alone – Real pet parents shared their wins and worries—and found guidance, not judgment.
💚 Catch the replay to shift from symptom-chasing to soul-nourishing pet care.
Would You Like to Join Our Next Public Q&A Webinar?
We hold them every LAST Friday of the month.
Sign up below to get notified about the next session.

Dr. Christina
Christina Chambreau, DVM, is an internationally known homeopathic veterinarian and associate editor of the Integrative Veterinary Care Journal, she’s written several books on animal healthcare.
After opening her own homeopathy veterinary practice in 1983, she founded the Academy Of Veterinary Homeopathy and was on the faculty of the National Center for Homeopathy Summer School for ten years.
Dr. Christina is also an integrative medicine adjunct faculty liaison for the Maryland Veterinary Technician Program and lectures on a wide array of topics including integrating holistic options into veterinary practices, as well as guidance on how to choose the best approaches to heal animals and sustainability.

Dr. Jeff
Jeffrey Feinman, BA, VMD, CVH, graduated in 1985 from the University of Pennsylvania and was Penn’s first veterinary dual-degree University Scholar, holding both molecular biology and veterinary degrees. He is the founder of HolisticActions.com and dedicated to pet parent empowerment.
Dr. Jeff is devoted to researching about how to harness the innate power of the individual using Vitality and Balance. He and his wonderful wife Amy live with Archie, a rescue pup, and a Rex cat named Tigger.
